PseudoPatient®
PseudoPatient® is a unique, personalized approach that optimizes patient safety and treatment outcomes by contributing to measures that minimize the risk of side-effects during brain radiotherapy.
Our innovation allows for an integrated evaluation of all treatment processes via a patient-specific, anatomically-exact model of real patient’s head and brain tissue. By applying all processes to the anatomically faithful replica, radiotherapy professionals can evaluate the whole treatment chain, identifying potential patient exposure to risk.
The critical demands in cranial radiotherapy applications (SRS/SRT) for accuracy and precision are met for the first time by PseudoPatient®: a truly personalized and individualized pre-treatment verification service.
PseudoPatient® advanced technology is internationally patented, FDA 510(k) cleared and ISO13485 certified.
The PseudoPatient® IC can accommodate any type(s) of detector or detectors the end-user would like, placed at any designated locations within the brain. This allows dosimetry tailored to the user’s needs and dosimeters availability. Placing detectors at designated locations also allows for dose measurements at the most dosimetrically demanding areas of the brain and the most critical clinical cases. In contrast, other commercially available solutions can accommodate inserts for dosimeters at limited pre-defined positions using selected dosimeters without any room for customizability/flexibility.
The PseudoPatient® 3D is used to verify third party treatment planning as well as radiation treatment chain for brain lesion radiation through the visualization of the 3D Dose pattern.
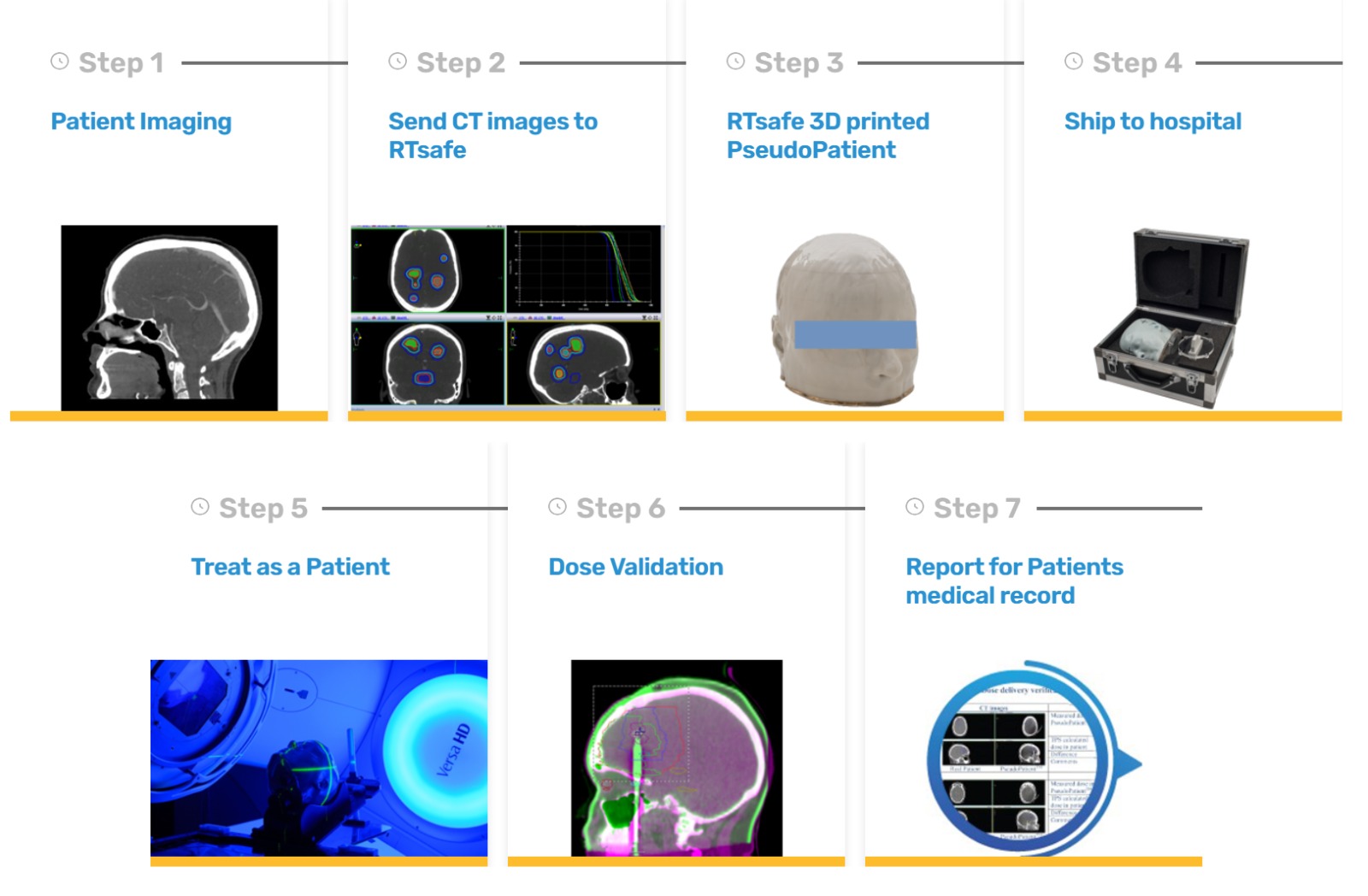
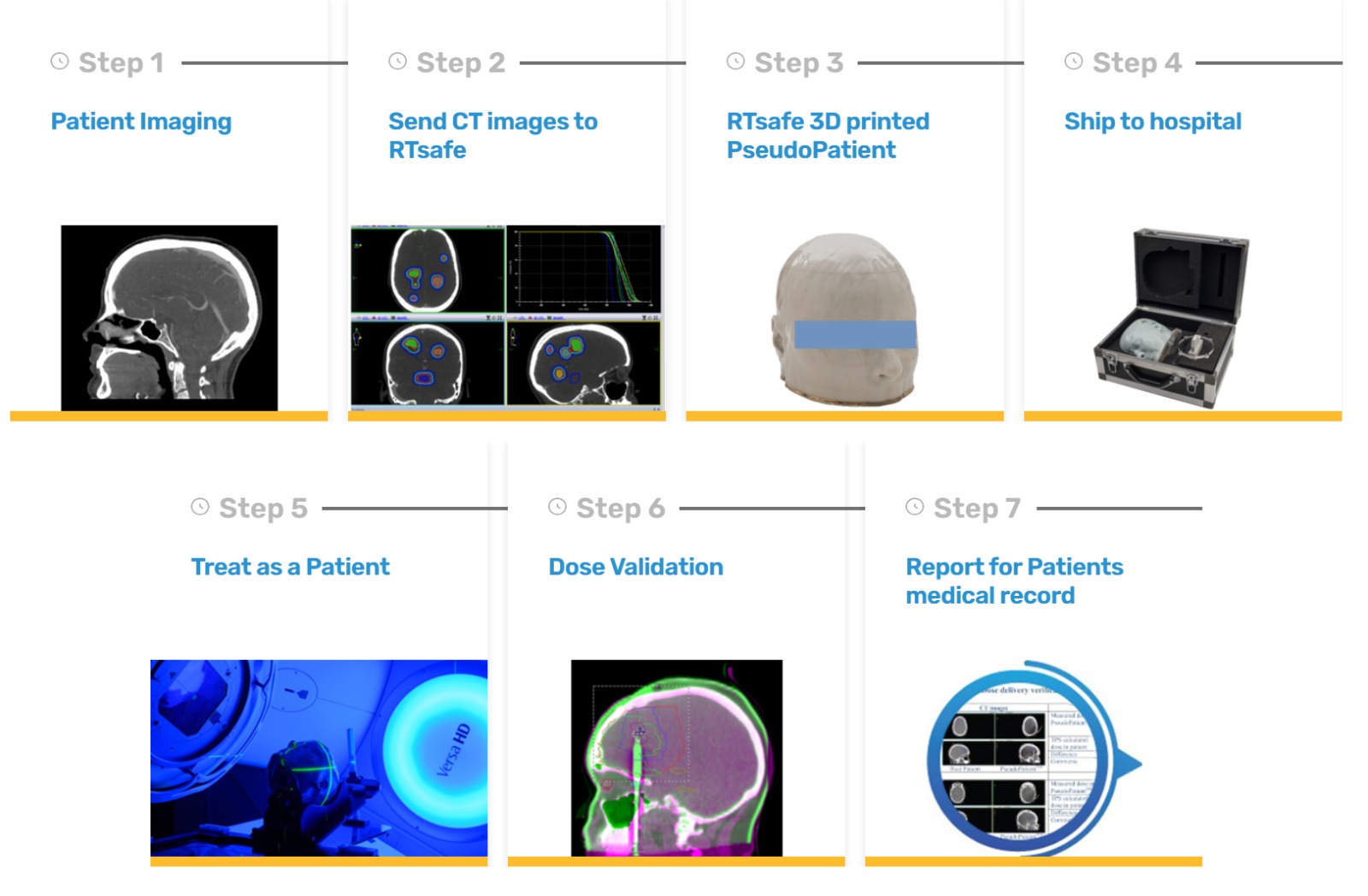
First, the CT scan of the patient is obtained and used to construct the exact replica of patient’s head. The final product is constructed from bone equivalent material and polymer gel as tissue mimicking material. Second, the CT-scan of the PseudoPatient® 3D is co-registered with the patient’s CT images using any third-party treatment planning system (TPS).
The physician and physicist shall create an irradiation plan, using department guidelines, and treat the phantom as the real patient in order to simulate the whole treatment chain. After irradiation the phantom has to be MR scanned using a clinical T2 weighted sequence (or a T2 parametric map).
These MR images depict the high dose areas of the dosimetric gel as darker than the low dose ones. After coregistering the TPS calculations and the MR images the user can qualitatively verify the geometric accuracy of the dose delivered to the phantom.
Key Features
- Exact anatomical replica of real patient’s anatomy.
- Direct measurements on anatomic regions of high interest (PTV, OAR). Providing options as High spatial resolution (of ~1mm³) 3D relative dosimetry. Absolute 2D film dosimetry. Absolute point dose measurements.
- End-to-end evaluation of all treatment processes.
- Medical record evidence of true treatment results under realistic conditions.
Intended for
Unique value-adds of PseudoPatient® are for:
- Patients: Treatment checked, approved, improved or rejected prior to real implementation. Potentially leading to better outcomes, lower side-effects, and higher quality of life.
- Clinicians: : Increased confidence in complex brain treatment delivery and total control of the process, Consultation tool for better doctor-patient communication.
- Physicists: Minimization of uncertainties. Individualized quality monitoring through real end-to-end pre-treatment testing.
- Clinics: Faster adoption of latest techniques, (such as SRS), leading to higher patient throughput and ROI, as well as data acquisition on individual treatment accuracy. Opportunity for data-driven continuous improvement and standardization. Differentiation and enhancement of clinic’s reputation through unique patient experience, aiming to address the specific individualized needs for maximized safety and efficacy.
PseudoPatient IC – How it works
PseudoPatient 3D – How it works
PseudoPatient vs other approaches
- The PseudoPatient ® phantom is an exact anatomical replica of the real patient. It is NOT an approximation, human-looking android.
- Availability of the real patient’s CT scan allows for more realistic contouring of anatomy at risk and target locations involved in intracranial SRS (e.g., brainstem, optic chiasm, etc.).
- Dose measurements can be implemented in prescribed regions of interest specifically for each case, achieving true end-to-end verification.
- The PseudoPatient® phantom can be filled with polymer gel covering the total brain-tissue volume, enabling high-fidelity 3D dose measurements (resolution of approximately 1mm3).